Formulary Exception Form
Formulary Exception Form - Most plans require that your doctor submit a. Web formulary exception prior authorization/medical necessity determination prescriber fax form only the prescriber may complete this form. Your doctor can go online and request a coverage decision for you. Select the list of exceptions for your plan. Web formulary exception/prior authorization request form expedited/urgent review requested: Please note that the prescription benefit and/or plan contract may exclude certain medications. Web formulary exception requests will be evaluated and a determination of coverage made utilizing all the following criteria: Web request rationale history of a medical condition, allergies or other pertinent information requiring the use of this medication: Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity limit) for a. Member’s eligibility to receive requested services (enrollment in the plan, prescription drug coverage, specific exclusions in member’s contract)
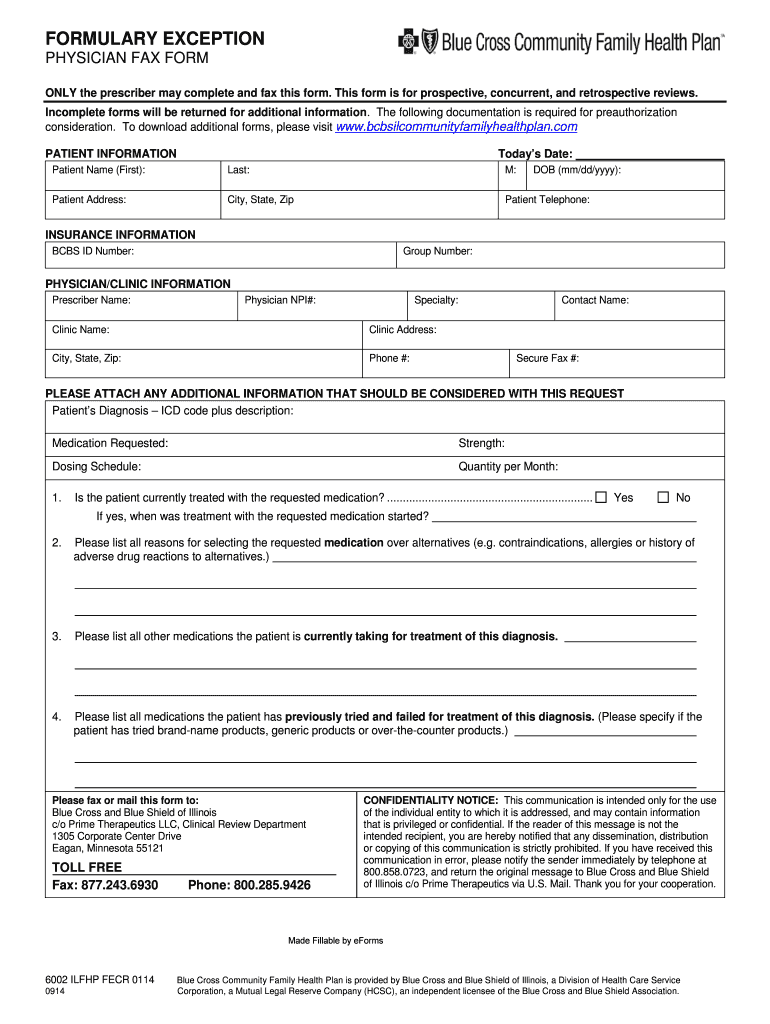
Incomplete forms will be returned for additional information. Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity limit) for a. Web formulary exception requests will be evaluated and a determination of coverage made utilizing all the following criteria: Web formulary exception request form formulary exception request this form may be used to request exceptions from the drug formulary, including drugs requiring prior authorization. The documents accompanying this transmission contain confidential health information that is legally privileged. Select the list of exceptions for your plan. Your doctor can go online and request a coverage decision for you. Most plans require that your doctor submit a. This form is for prospective, concurrent, and retrospective reviews. Web formulary exception prior authorization/medical necessity determination prescriber fax form only the prescriber may complete this form.
Web formulary exception requests will be evaluated and a determination of coverage made utilizing all the following criteria: Select the list of exceptions for your plan. The documents accompanying this transmission contain confidential health information that is legally privileged. Web when faced with uncovered medications, you have an option to file a formulary exception with your insurance to request that they allow you coverage for the medication. Start saving time today by filling out this prior. Web complete this form to request a formulary exception, tiering exception, prior authorization or reimbursement. Web formulary exception/prior authorization request form expedited/urgent review requested: This form is for prospective, concurrent, and retrospective reviews. Web formulary exception prior authorization/medical necessity determination prescriber fax form only the prescriber may complete this form. Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity limit) for a.
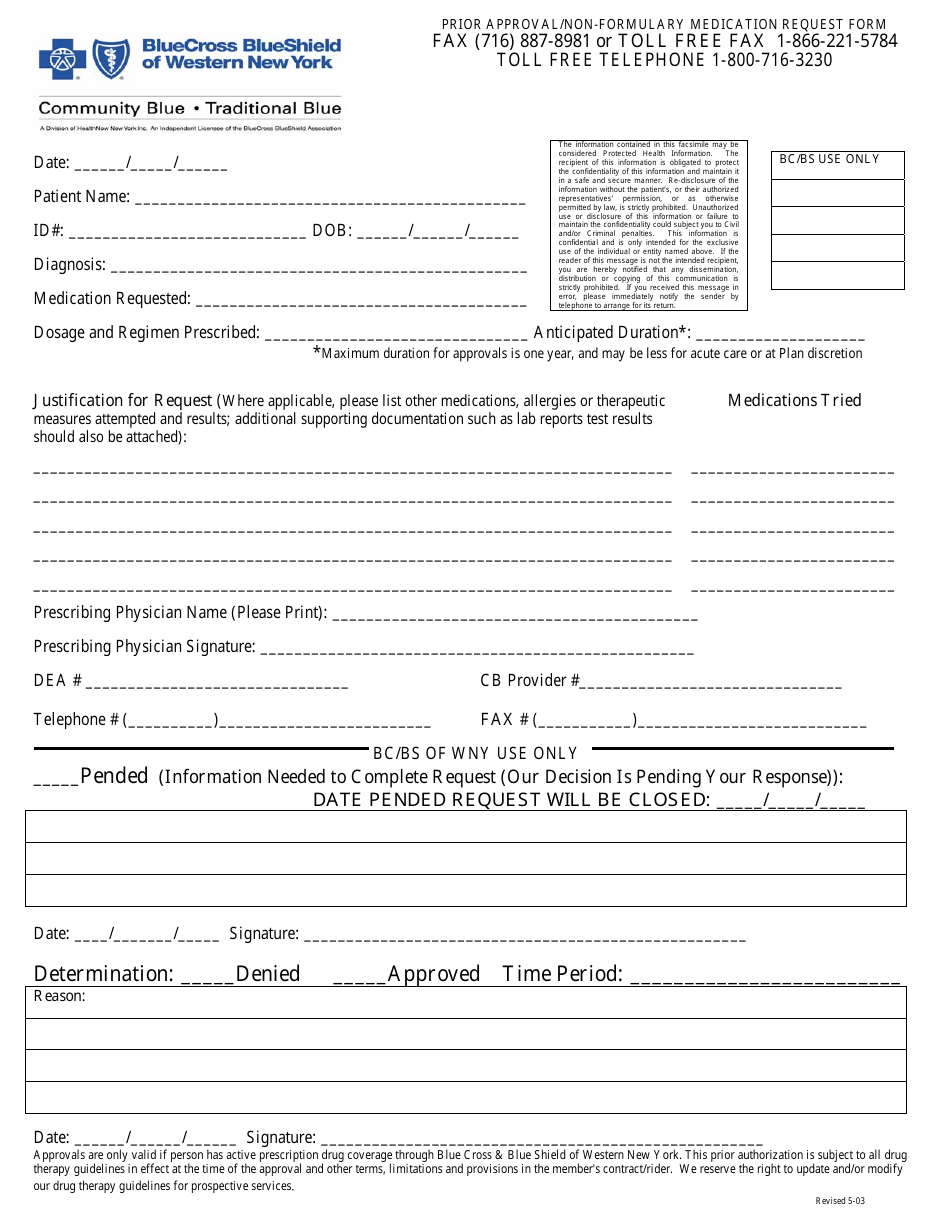
New York Prior Approval/Nonformulary Medication Request Form Blue
Start saving time today by filling out this prior. Incomplete forms will be returned for additional information. Web formulary exception request form formulary exception request this form may be used to request exceptions from the drug formulary, including drugs requiring prior authorization. This form is for prospective, concurrent, and retrospective reviews. The documents accompanying this transmission contain confidential health information.
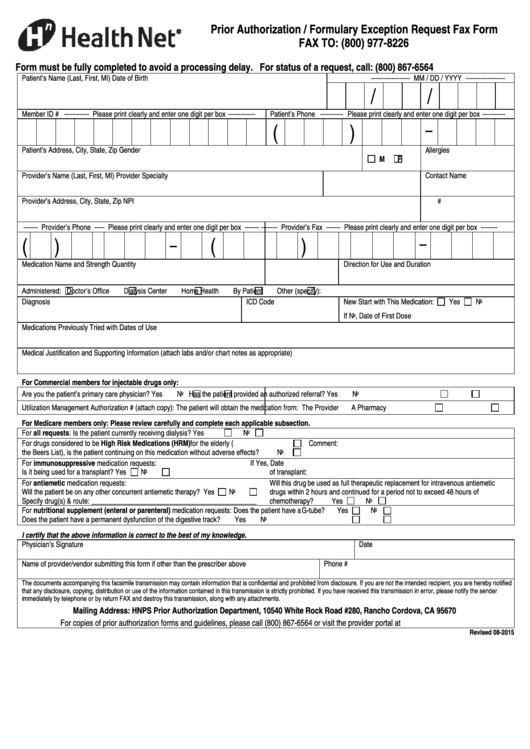
Health Net Prior Authorization / Formulary Exception Request Fax Form
Web formulary exception/prior authorization request form expedited/urgent review requested: This form is for prospective, concurrent, and retrospective reviews. Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity limit) for a. Select.
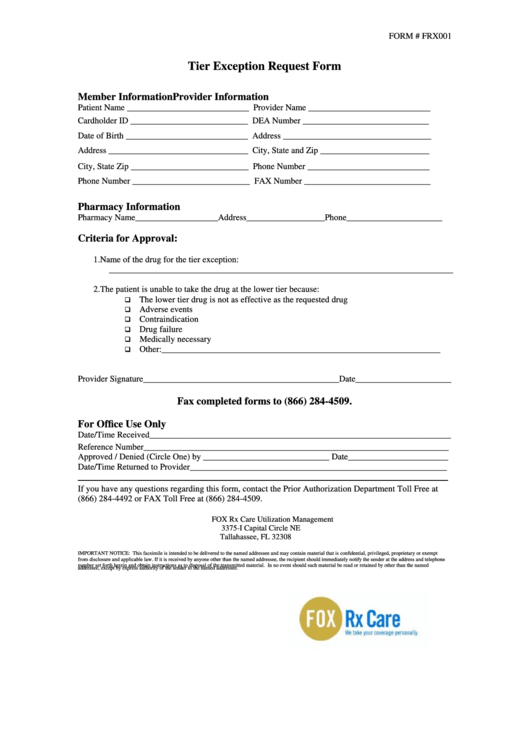
Form Frx001 Tier Exception Request Form printable pdf download
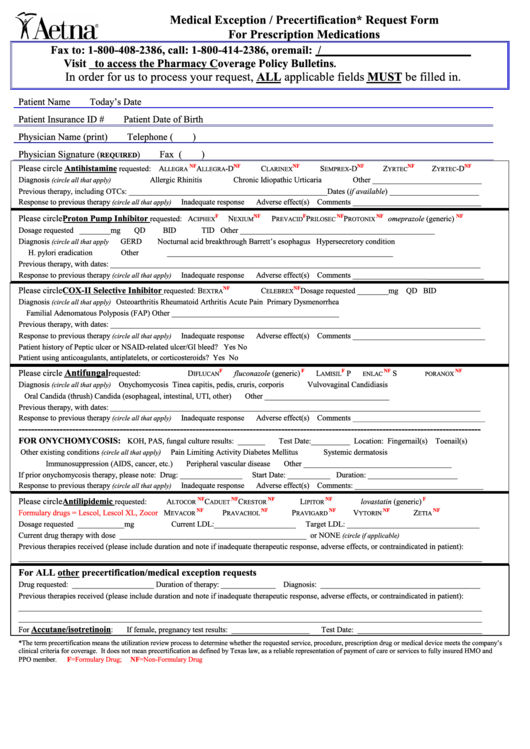
Web formulary exception prior authorization/medical necessity determination prescriber fax form only the prescriber may complete this form. Start saving time today by filling out this prior. This form is for prospective, concurrent, and retrospective reviews. Web request rationale history of a medical condition, allergies or other pertinent information requiring the use of this medication: Web a formulary exception should be.
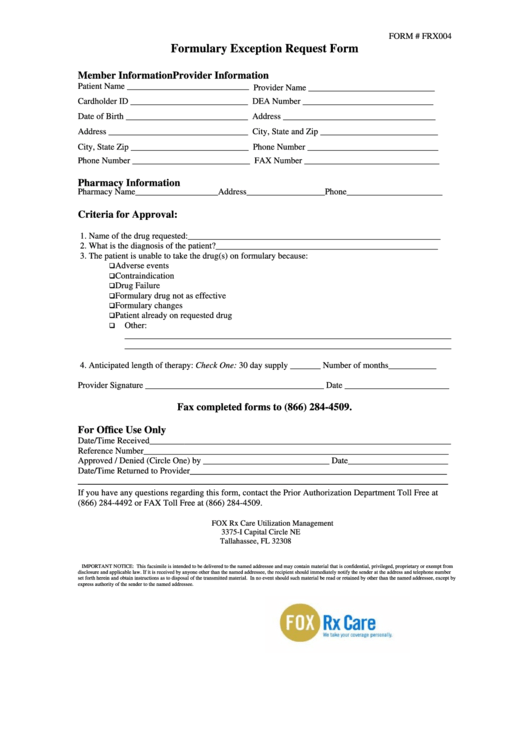
Form Frx004 Formulary Exception Request Form printable pdf download
By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web complete this form to request a formulary exception, tiering exception, prior authorization or reimbursement. Web formulary exception requests will be evaluated and a determination of.
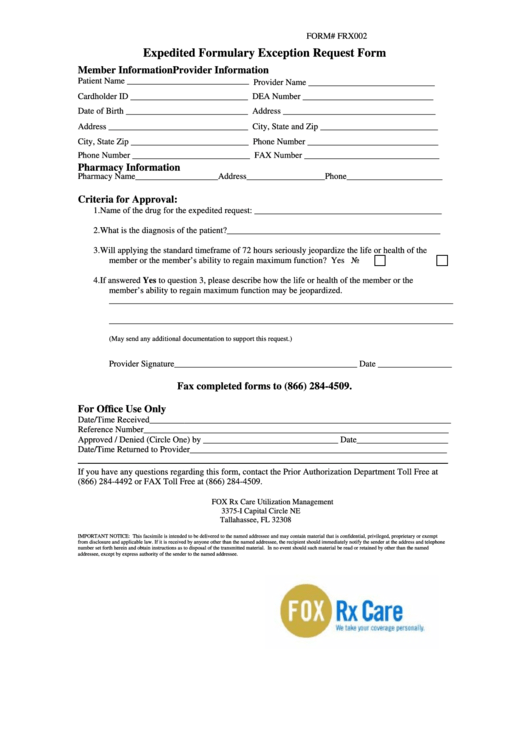
Form Frx002 Expedited Formulary Exception Request Form printable pdf
Web request rationale history of a medical condition, allergies or other pertinent information requiring the use of this medication: By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Web formulary exception/prior authorization request form expedited/urgent.
FORMULARY EXCEPTION PHYSICIAN FAX FORM Fill Out and Sign Printable
Your doctor can go online and request a coverage decision for you. Incomplete forms will be returned for additional information. Web request rationale history of a medical condition, allergies or other pertinent information requiring the use of this medication: Please note that the prescription benefit and/or plan contract may exclude certain medications. Web formulary exception prior authorization/medical necessity determination prescriber.
Anthem Medicare Advantage Disenrollment Form Form Resume Examples
Most plans require that your doctor submit a. Incomplete forms will be returned for additional information. This form is for prospective, concurrent, and retrospective reviews. Web formulary exception requests will be evaluated and a determination of coverage made utilizing all the following criteria: Web formulary exception request form formulary exception request this form may be used to request exceptions from.
Bcbs Formulary Exception Form Fill Online, Printable, Fillable, Blank
Web when faced with uncovered medications, you have an option to file a formulary exception with your insurance to request that they allow you coverage for the medication. By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain.
Aetna Medical Exception / Precertification Request Form printable pdf
Please note that the prescription benefit and/or plan contract may exclude certain medications. Web formulary exception/prior authorization request form expedited/urgent review requested: Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity.
Sample Prime Therapeutics Prior Authorization Form Sample Templates
Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity limit) for a. Start saving time today by filling out this prior. This form is for prospective, concurrent, and retrospective reviews. Web.
Web Formulary Exception/Prior Authorization Request Form Expedited/Urgent Review Requested:
Incomplete forms will be returned for additional information. Web complete this form to request a formulary exception, tiering exception, prior authorization or reimbursement. Web a formulary exception should be requested to obtain a part d drug that is not included on a plan sponsor's formulary, or to request to have a utilization management requirement waived (e.g., step therapy, prior authorization, quantity limit) for a. Your doctor can go online and request a coverage decision for you.
Web Formulary Exception Request Form Formulary Exception Request This Form May Be Used To Request Exceptions From The Drug Formulary, Including Drugs Requiring Prior Authorization.
Select the list of exceptions for your plan. The documents accompanying this transmission contain confidential health information that is legally privileged. This form is for prospective, concurrent, and retrospective reviews. Web request rationale history of a medical condition, allergies or other pertinent information requiring the use of this medication:
Most Plans Require That Your Doctor Submit A.
Start saving time today by filling out this prior. Member’s eligibility to receive requested services (enrollment in the plan, prescription drug coverage, specific exclusions in member’s contract) Web when faced with uncovered medications, you have an option to file a formulary exception with your insurance to request that they allow you coverage for the medication. Web formulary exception prior authorization/medical necessity determination prescriber fax form only the prescriber may complete this form.
Web Formulary Exception Requests Will Be Evaluated And A Determination Of Coverage Made Utilizing All The Following Criteria:
By checking this box and signing below, i certify that applying the standard review time frame may seriously jeopardize the life or health of the patient or the patient’s ability to regain maximum function. Please note that the prescription benefit and/or plan contract may exclude certain medications.