Highmark Bcbs Pennsylvania Prior Authorization Form
Highmark Bcbs Pennsylvania Prior Authorization Form - Durable medical equipment/medical injectable drugs/outpatient procedures: Web electronic forms are submitted directly to highmark via this website. † agents used for fibromyalgia (e.g. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. Web dificid prior authorization form. Web prior authorization request form highmark health options is an independent licensee of the blue cross blue shield association, an association of independent blue cross blue. Using navinet is the preferred way to request prior authorization/notification from nia. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional. All references to highmark in this document are references to highmark inc. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization:
Web covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web home health the ordering provider is typically responsible for obtaining authorizations for the procedures/services included on the list of procedures/dme requiring. Extended release opioid prior authorization form. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Web dificid prior authorization form. † agents used for fibromyalgia (e.g. Highmark blue cross blue shield, highmark choice company, highmark health. Web prior authorization request form highmark health options is an independent licensee of the blue cross blue shield association, an association of independent blue cross blue. If you do not yet. Web electronic forms are submitted directly to highmark via this website.
D/b/a highmark blue shield and/or to one or. Using navinet is the preferred way to request prior authorization/notification from nia. Web covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. All references to highmark in this document are references to highmark inc. Or certain of its affiliated blue companies also serve blue cross blue shield members in 29 counties in western pennsylvania, 13 counties in. Web highmark transitioning from navinet to availity starting in october 2023. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. Complete and fax all requested information below including any supporting documentation as applicable to highmark health. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization: Web state of delaware and 8 counties in western new york.
Amerigroup Nj Prior Authorization Form Form Resume Examples EY39YQGn32
Web covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional. You may need.
Blue cross blue shield pennsylvania highmark availity
Web covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. Covermymeds automates the prior authorization (pa). Web electronic forms are submitted directly to highmark via this website. You may need to upload documentation/provide additional research during parts of this form. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data,.
Gallery of Highmark Bcbs Medication Prior Authorization form Lovely
Extended release opioid prior authorization form. Using navinet is the preferred way to request prior authorization/notification from nia. Web dificid prior authorization form. Covermymeds automates the prior authorization (pa). Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form.
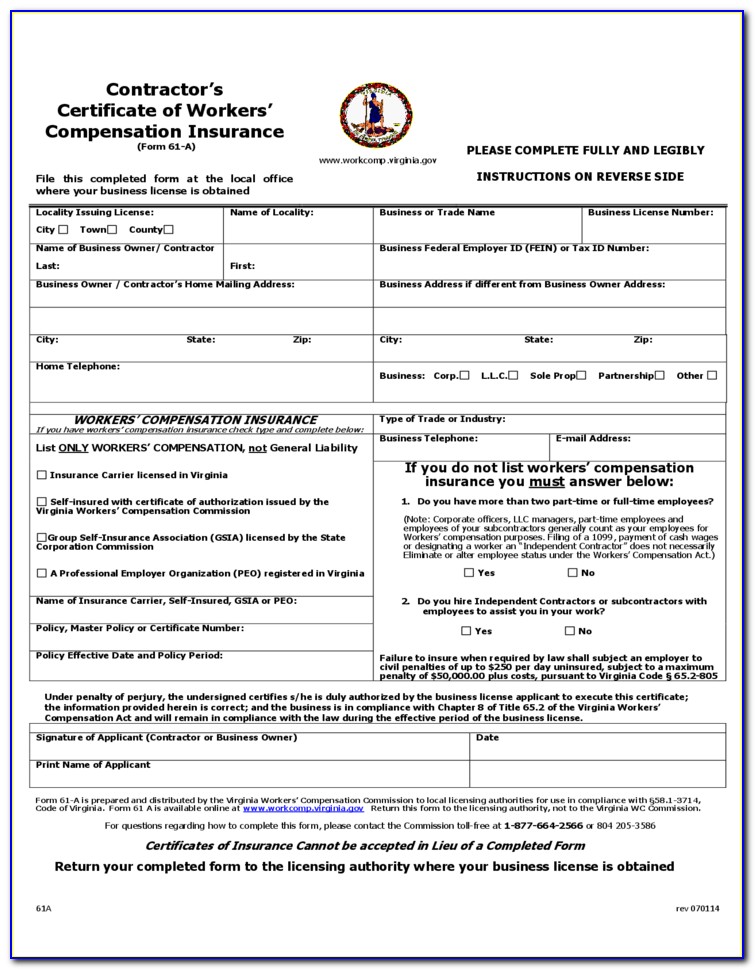
Bcbs Prior Authorization Form Maryland Form Resume Examples Yqlkmob5aj
Web dificid prior authorization form. Review the prior authorizations section of the provider manual. Highmark blue cross blue shield, highmark choice company, highmark health. Durable medical equipment/medical injectable drugs/outpatient procedures: Extended release opioid prior authorization form.
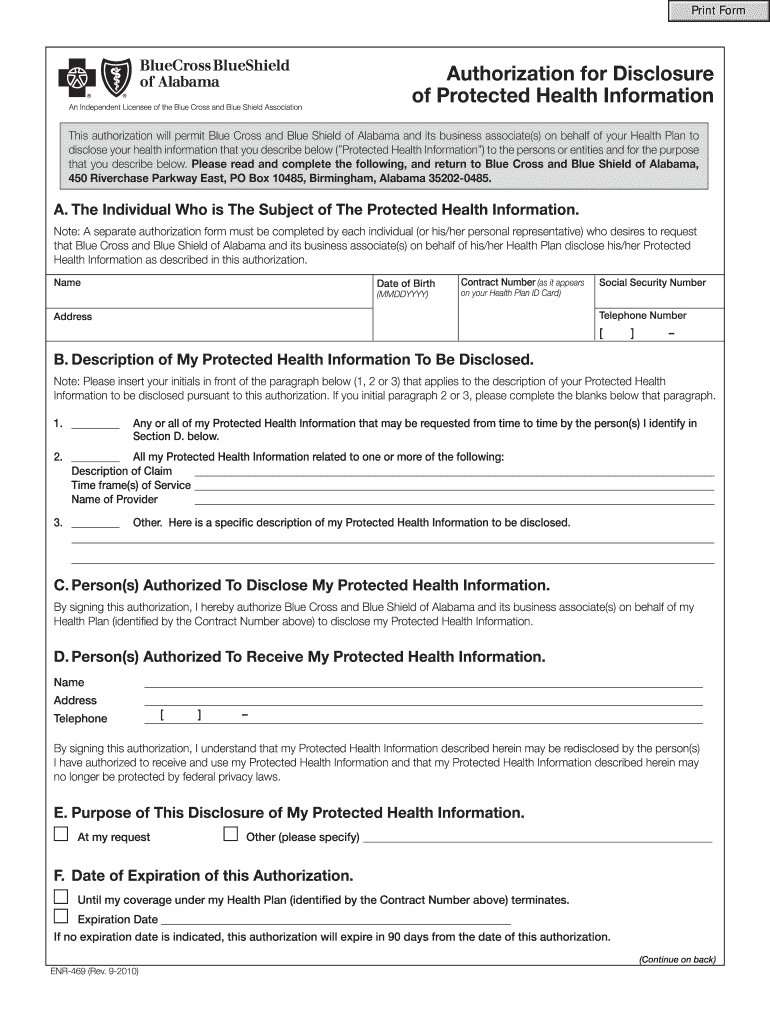
Bcbs of alabama authorization for disclosure of protected health
Web covermymeds is highmark blue shield prior authorization forms’s preferred method for receiving epa requests. If you do not yet. Extended release opioid prior authorization form. Durable medical equipment/medical injectable drugs/outpatient procedures: Web how to request prior authorization/notification.
Carefirst bcbs reimbursement form
Web electronic forms are submitted directly to highmark via this website. Web how to request prior authorization/notification. Web independent blue cross blue shield plans. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. † agents used for fibromyalgia (e.g.
Bcbs Highmark Login
Web prior authorization request form highmark health options is an independent licensee of the blue cross blue shield association, an association of independent blue cross blue. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. Highmark blue cross blue shield, highmark choice company, highmark health. Web state of delaware and.
Bcbs Prior Auth Forms To Print Fill Online, Printable, Fillable
Complete and fax all requested information below including any supporting documentation as applicable to highmark health. D/b/a highmark blue shield and/or to one or. You may need to upload documentation/provide additional research during parts of this form. Extended release opioid prior authorization form. All references to highmark in this document are references to highmark inc.
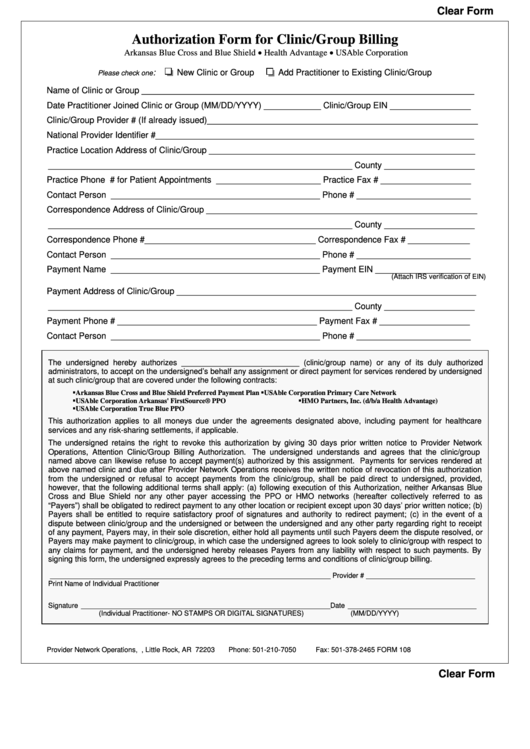
Fillable Bcbs Authorization Form For Clinic/group Billing printable pdf
Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. Web home health the ordering provider is typically responsible for obtaining authorizations for the procedures/services included on the list of procedures/dme requiring. Durable medical equipment/medical injectable drugs/outpatient procedures: Covermymeds automates the prior authorization (pa). Using navinet is the preferred way to.
42 Best Bcbs Nc Prior Authorization forms for
D/b/a highmark blue shield and/or to one or. Web prior authorization request form highmark health options is an independent licensee of the blue cross blue shield association, an association of independent blue cross blue. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. If you do not yet. Covermymeds automates.
Web Prior Authorization Request Form Highmark Health Options Is An Independent Licensee Of The Blue Cross Blue Shield Association, An Association Of Independent Blue Cross Blue.
Web highmark transitioning from navinet to availity starting in october 2023. Web independent blue cross blue shield plans. If you do not yet. Highmark blue cross blue shield, highmark choice company, highmark health.
Complete And Fax All Requested Information Below Including Any Supporting Documentation As Applicable To Highmark Health.
Web home health the ordering provider is typically responsible for obtaining authorizations for the procedures/services included on the list of procedures/dme requiring. Web state of delaware and 8 counties in western new york. Extended release opioid prior authorization form. All references to highmark in this document are references to highmark inc.
Web Prior Authorization Below Is A List Of Common Drugs And/Or Therapeutic Categories That Require Prior Authorization:
Using navinet is the preferred way to request prior authorization/notification from nia. Covermymeds automates the prior authorization (pa). Web dificid prior authorization form. † agents used for fibromyalgia (e.g.
Web How To Request Prior Authorization/Notification.
Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional. Web pharmacy prior authorization forms addyi prior authorization form blood disorders medication request form cgrp inhibitors medication request form. Durable medical equipment/medical injectable drugs/outpatient procedures: Review the prior authorizations section of the provider manual.