Hmsa Prior Authorization Form
Hmsa Prior Authorization Form - To make an appropriate determination, providing the most accurate diagnosis for the use of the Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. Web standard request for medicare and medicaid plans: Web utilization management (um) department prior authorization request phone number: To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. _ patient information last name first name phone number gender m f date of birth member id # (if known): Decisions & notification are made within 15calendar days* expedited request (md,. Web hawaii medicaid prior authorization form hawaii standardized prescription drug prior authorization form* request date:
Decisions & notification are made within 15calendar days* expedited request (md,. Contact name (first, last) member. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Hmsa medical management department p. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans:
Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web hawaii medicaid prior authorization form hawaii standardized prescription drug prior authorization form* request date: Hmsa medical management department p. Fast pass providers aren’t required to request prior authorization. Web utilization management (um) department prior authorization request phone number: This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. To make an appropriate determination, providing the most accurate diagnosis for the use of the This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization.
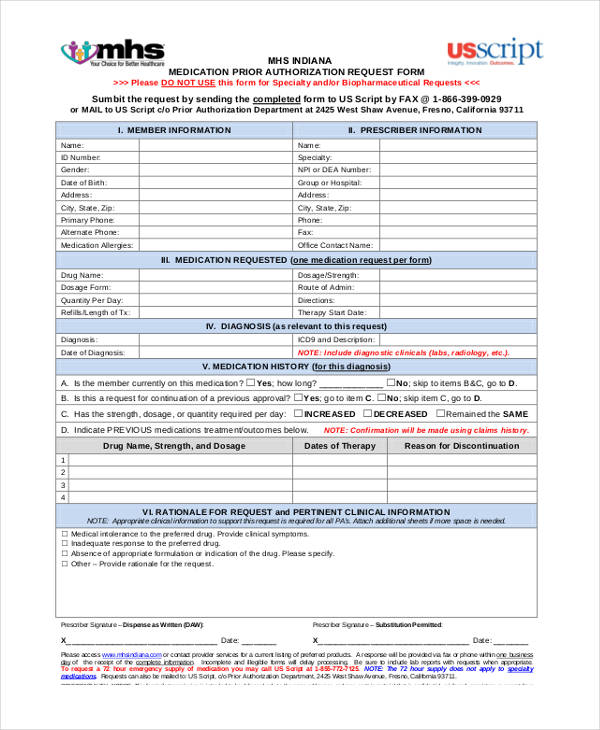
ads/responsive.txt Health Net Prior Authorization form for Medication
This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. Requesting prior authorization • providers are encouraged to use radmd.com to.
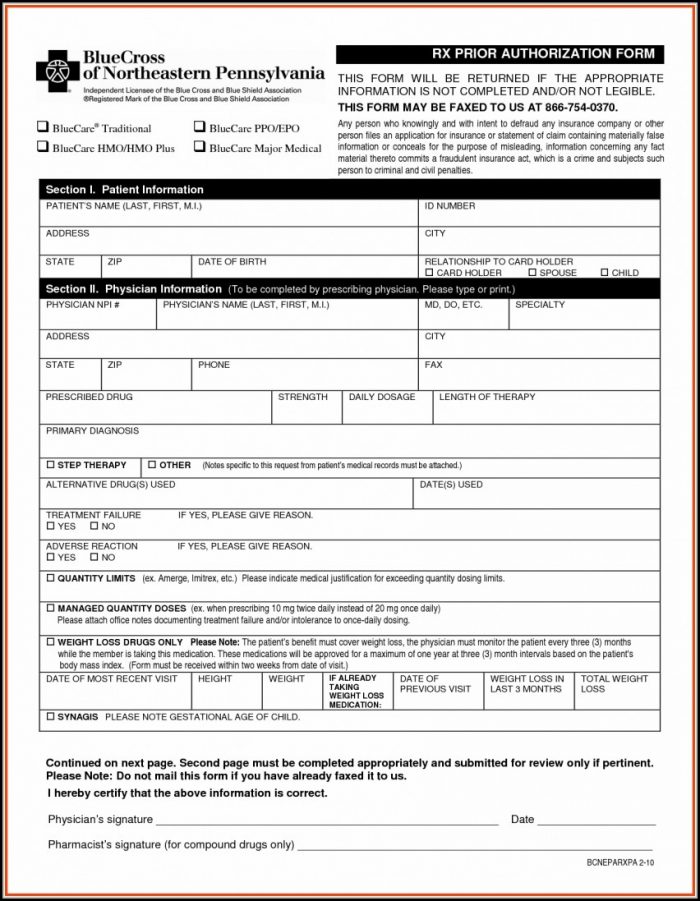
Express Scripts Prior Authorization Form Medicare Part D Form
To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. To make an appropriate determination, providing the most accurate diagnosis.
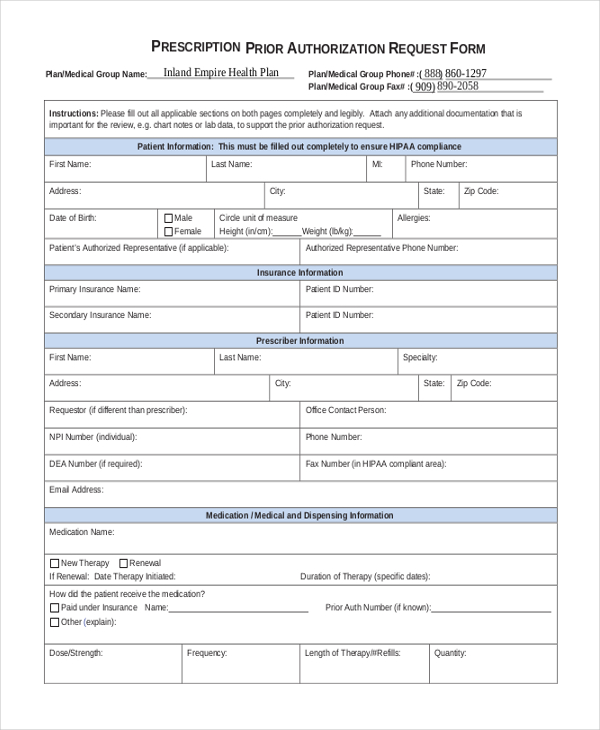
FREE 13+ Prior Authorization Forms in PDF MS Word
Web hawaii medicaid prior authorization form hawaii standardized prescription drug prior authorization form* request date: This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans: Requesting prior authorization • providers are encouraged to use radmd.com to request.
Medco Prior Authorization Form Form Resume Examples XV8oMxYKzD
Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. Web utilization management (um) department prior authorization request phone number: _ patient information last name first name phone number gender m f date of.
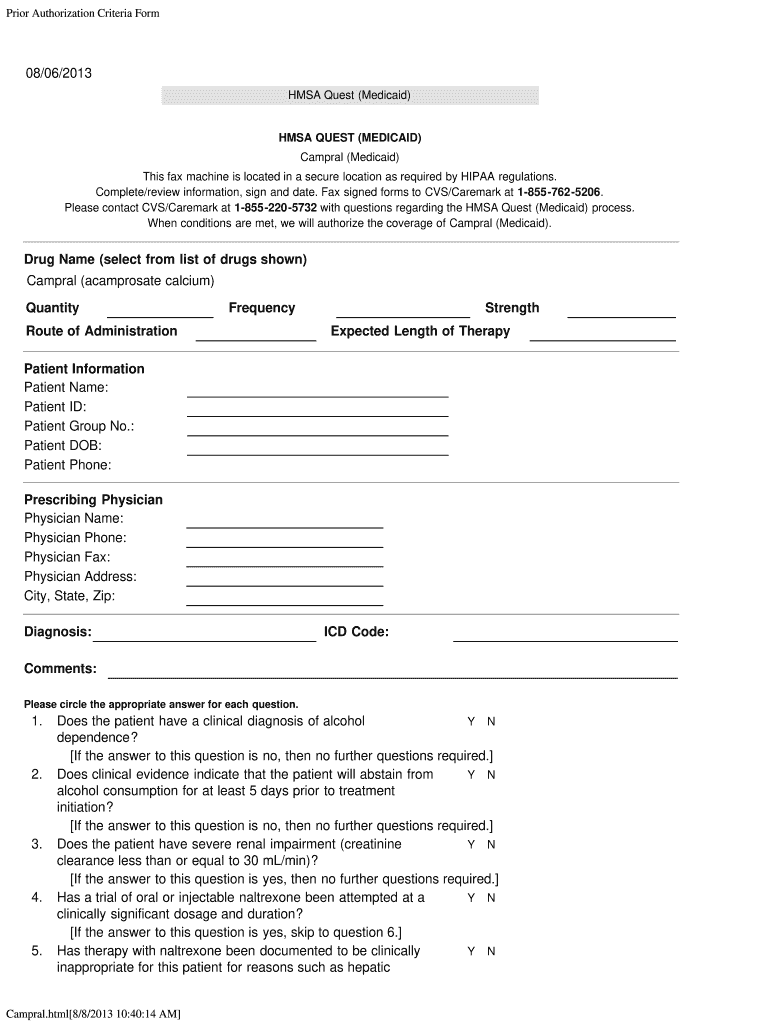
Authorization Medicaid Campral Fill Out and Sign Printable PDF
To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies..
Ach Payment Authorization Form Template Template 2 Resume Examples
Contact name (first, last) member. Hmsa medical management department p. Web utilization management (um) department prior authorization request phone number: To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization.
Hmsa Medicaid Form Request Fill Online, Printable, Fillable, Blank
Hmsa medical management department p. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. Fast pass providers aren’t required to request prior authorization. Decisions & notification are made within 15calendar days* expedited request (md,. This standardized form is.
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web utilization management (um) department prior authorization request phone number:.
REQUEST FOR MEDICAL AUTHORIZATION in Word and Pdf formats
This standardized form is used for a general request for hmsa all lines of business when no other precertification request form applies. This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web.
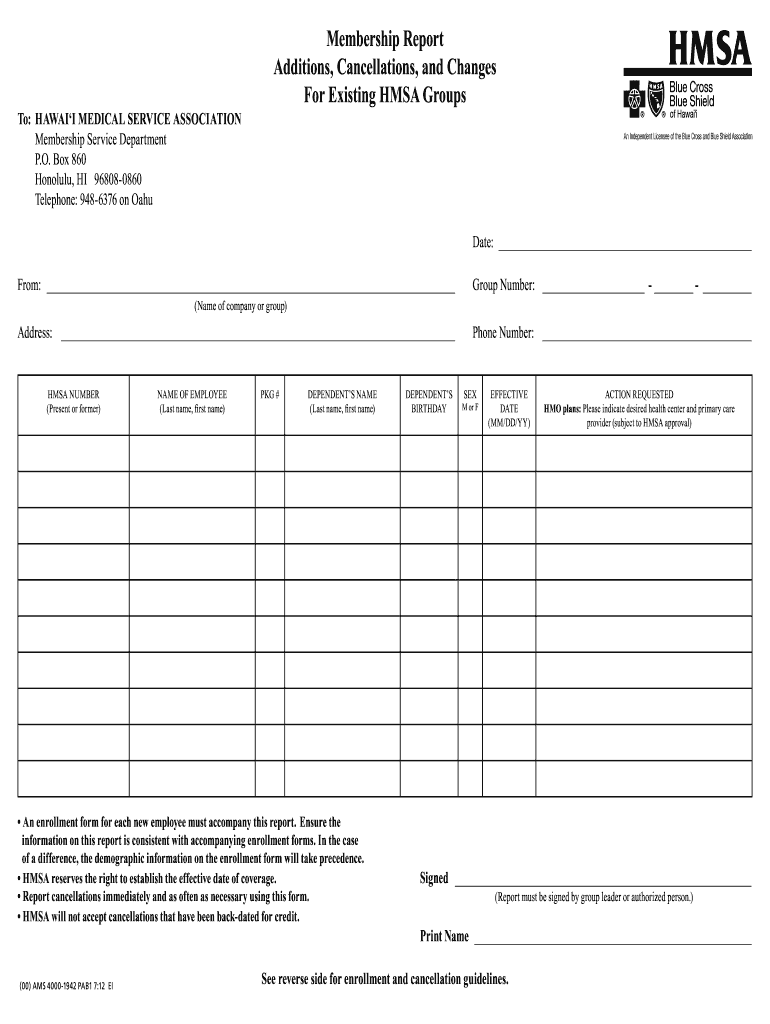
Hmsa Membership Report Form Fill Out and Sign Printable PDF Template
To make an appropriate determination, providing the most accurate diagnosis for the use of the To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Requesting prior authorization • providers are encouraged to use radmd.com to request prior authorization. Web this patient’s benefit plan requires prior authorization for certain medications in.
This Standardized Form Is Used For A General Request For Hmsa All Lines Of Business When No Other Precertification Request Form Applies.
To make an appropriate determination, providing the most accurate diagnosis for the use of the Web standard request for medicare and medicaid plans: Decisions & notification are made within 15calendar days* expedited request (md,. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered.
Contact Name (First, Last) Member.
Web utilization management (um) department prior authorization request phone number: Hmsa medical management department p. Decision & notification are made within 14calendar days* for hmsa commercial, federal and eutf plans: Fast pass providers aren’t required to request prior authorization.
Web Hawaii Medicaid Prior Authorization Form Hawaii Standardized Prescription Drug Prior Authorization Form* Request Date:
This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this standardized prior authorization request form can be used for most prior authorization requests and use across all four health plans, including alohacare, hmsa, 'ohana health plan, and united healthcare. _ patient information last name first name phone number gender m f date of birth member id # (if known): To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary.
Requesting Prior Authorization • Providers Are Encouraged To Use Radmd.com To Request Prior Authorization.
This patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered.