Molina Medicaid Prior Authorization Form
Molina Medicaid Prior Authorization Form - Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. Medicaid prior authorization annual review change log. • current (up to 6 months), adequate patient history related to the requested. Molina healthcare prior authorization request form and instructions. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Molina healthcare prior authorization request form and instructions. Add or close a location. The forms are also available on the frequently used forms page. If prior authorization is needed for a certain service, your provider must get it before giving you the service. Change office location, hours, phone, fax, or email.
Items on this list will only be dispensed after prior authorization from molina healthcare. The forms are also available on the frequently used forms page. Medicaid prior authorization annual review change log. Change office location, hours, phone, fax, or email. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Add or close a location. Web what are prior authorizations? It is needed before you can get certain services or drugs. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Molina healthcare prior authorization request form and instructions.
Behavioral health respite services pa reference guide. Items on this list will only be dispensed after prior authorization from molina healthcare. Molina healthcare prior authorization request form and instructions. • current (up to 6 months), adequate patient history related to the requested. Please click the links below to view documents related to prior authorization requirements. Molina healthcare prior authorization request form and instructions. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. Add or terminate a provider. It is needed before you can get certain services or drugs.
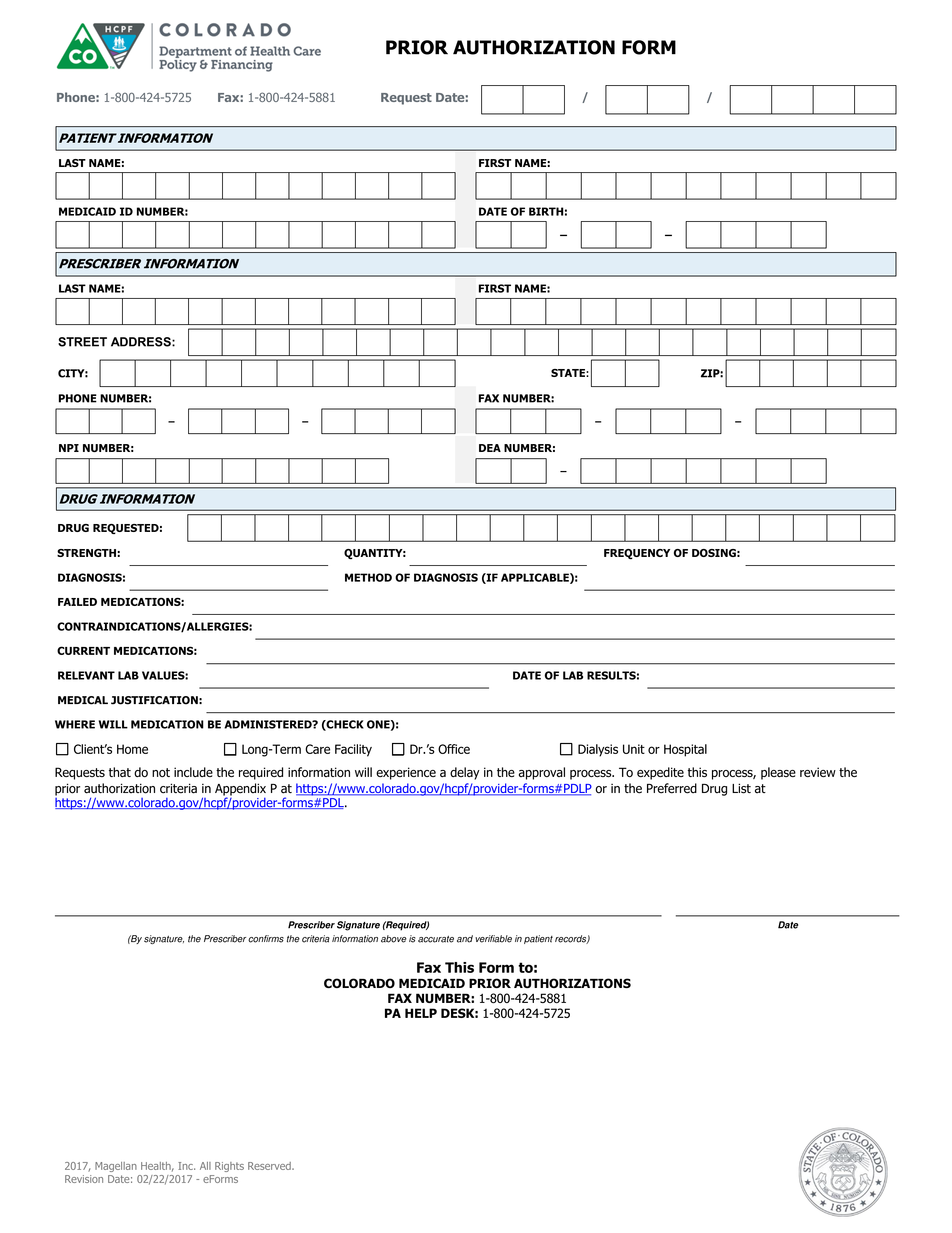
Free Colorado Medicaid Prior (Rx) Authorization Form PDF eForms
Behavioral health respite services pa reference guide. Add or close a location. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Web what are prior authorizations? Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax.
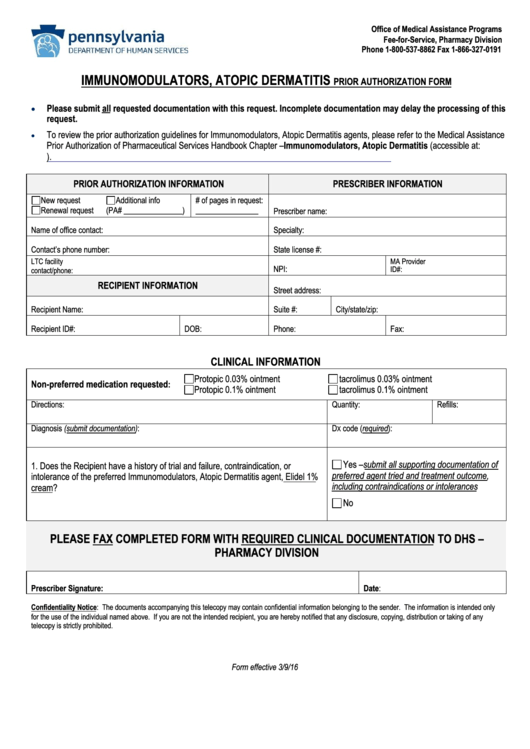
157 Prior Authorization free to download in PDF
Add or terminate a provider. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Molina healthcare prior authorization request form and instructions. It is needed before you can get certain services or drugs. • current (up to 6 months), adequate patient history related to the requested.
Prior Authorization Washington State Local Health Insurance CHPW
Add or terminate a provider. Please click the links below to view documents related to prior authorization requirements. Items on this list will only be dispensed after prior authorization from molina healthcare. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Behavioral health respite services.
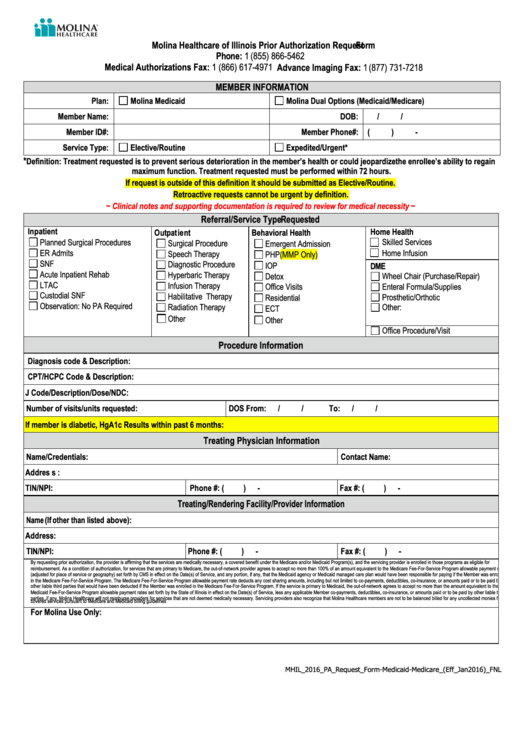
Molina Healthcare Of Illinois Prior Authorization Request printable pdf
Behavioral health respite services pa reference guide. Web what are prior authorizations? The forms are also available on the frequently used forms page. Medicaid prior authorization annual review change log. Web prior authorization is not a guarantee of payment for services.
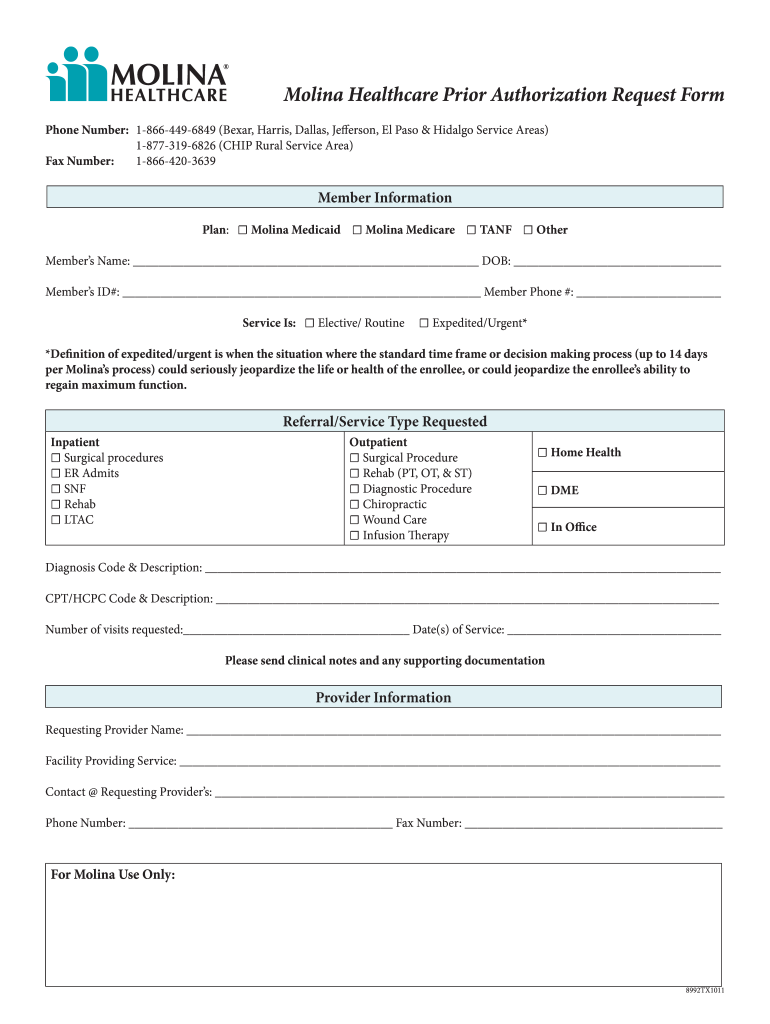
Molina Prior Authorization Form 2021 Fill Online, Printable, Fillable
Molina healthcare prior authorization request form and instructions. It is needed before you can get certain services or drugs. Web what are prior authorizations? Change office location, hours, phone, fax, or email. Please click the links below to view documents related to prior authorization requirements.
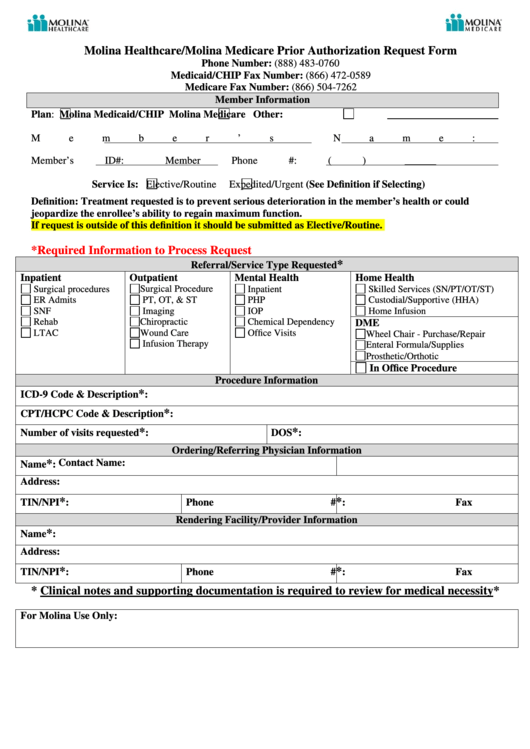
Molina Healthcare/molina Medicare Prior Authorization Request Form
• current (up to 6 months), adequate patient history related to the requested. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. Items on this list will only be dispensed after prior authorization from molina healthcare. Molina healthcare prior authorization request form and instructions. Add or close a location.
MOLINA HEALTHCARE, INC. FORM 8K EX99.1 September 16, 2011
• current (up to 6 months), adequate patient history related to the requested. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Change office location, hours, phone, fax, or email. Web what are prior authorizations? Behavioral health respite services pa reference guide.
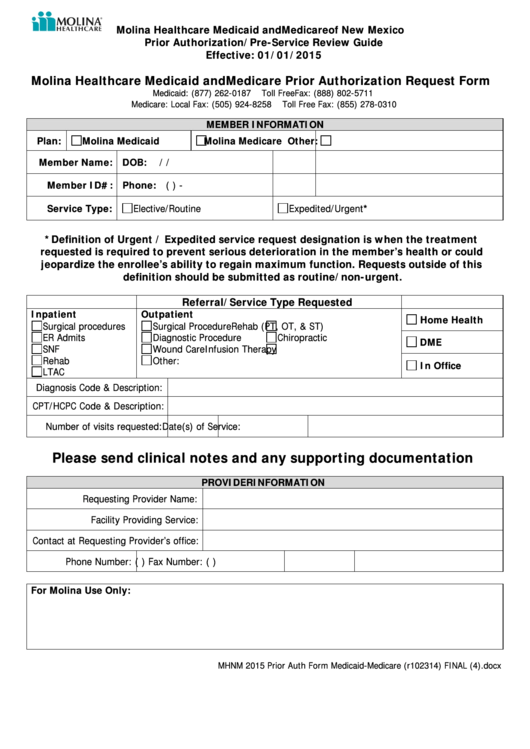
Molina Healthcare Medicaid And Medicare Prior Authorization Request
If prior authorization is needed for a certain service, your provider must get it before giving you the service. Web prior authorization is not a guarantee of payment for services. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: It is needed before you can.
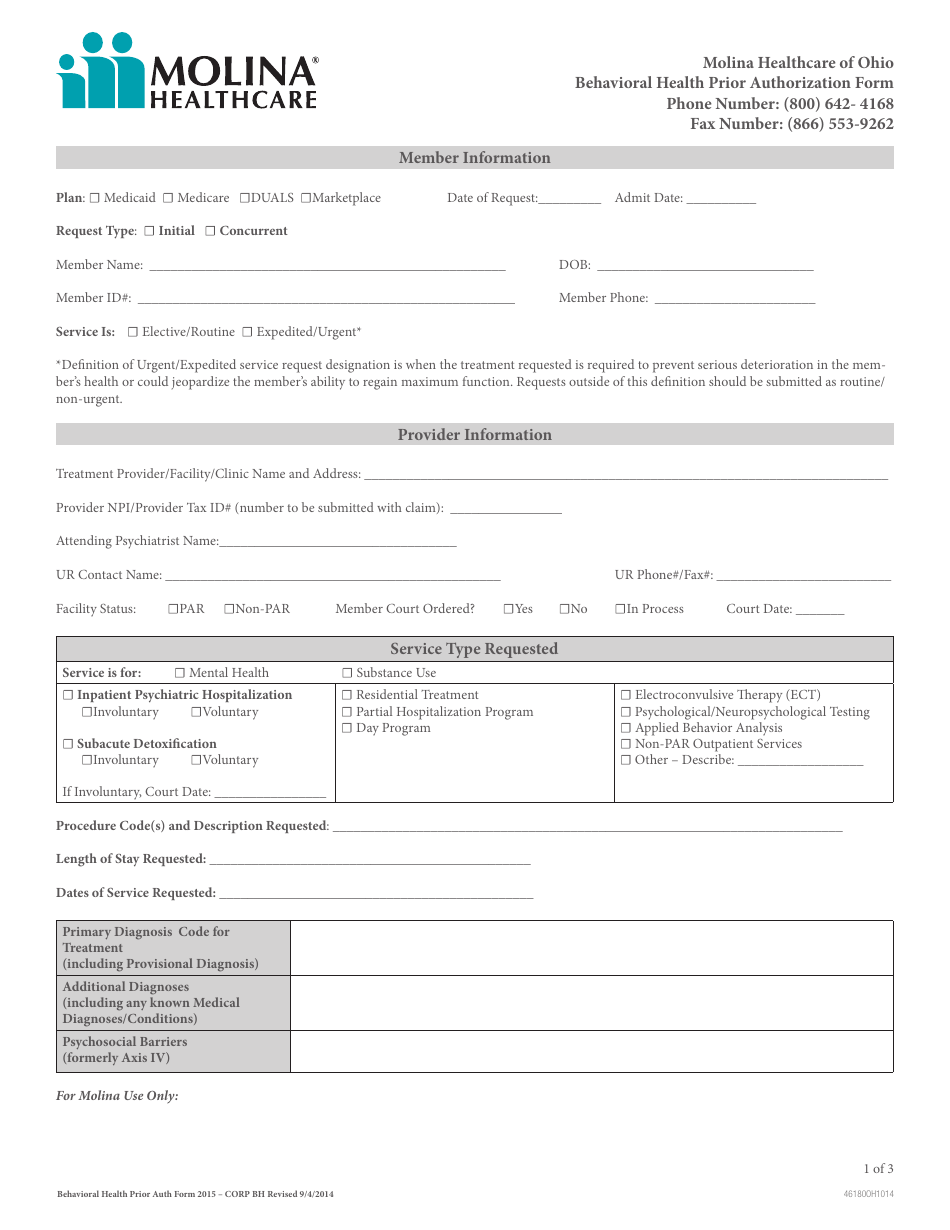
Ohio Behavioral Health Prior Authorization Molina Healthcare Download
Medicaid prior authorization annual review report. Molina healthcare prior authorization request form and instructions. If prior authorization is needed for a certain service, your provider must get it before giving you the service. It is needed before you can get certain services or drugs. Add or terminate a provider.
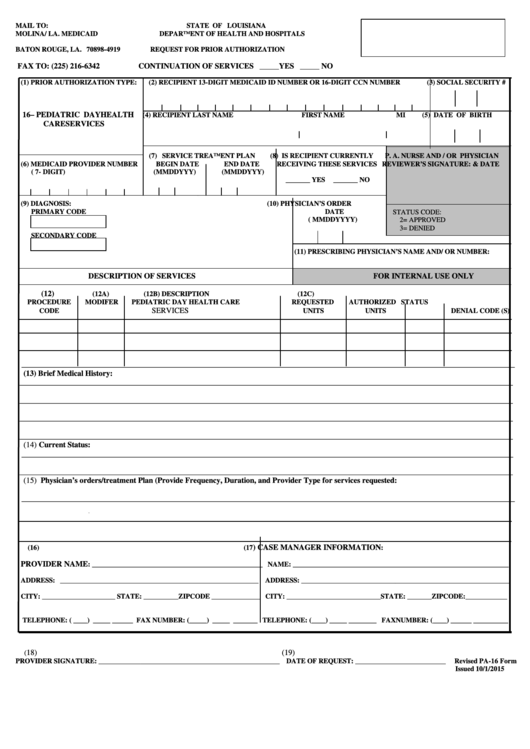
Prior Authorization Form (Pa16) Molina / La. Medicaid printable pdf
It is needed before you can get certain services or drugs. Web all general/physical health prior authorization requests can be submitted via the availity essentials provider portal or via fax. Behavioral health respite services pa reference guide. Items on this list will only be dispensed after prior authorization from molina healthcare. Prior authorization is when your provider gets approval from.
Medicaid Prior Authorization Annual Review Report.
Web we welcome your feedback and look forward to supporting all your efforts to provide quality care. Molina healthcare prior authorization request form and instructions. Medicaid prior authorization annual review change log. Web what are prior authorizations?
Web All General/Physical Health Prior Authorization Requests Can Be Submitted Via The Availity Essentials Provider Portal Or Via Fax.
It is needed before you can get certain services or drugs. Molina healthcare prior authorization request form and instructions. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Behavioral health respite services pa reference guide.
Please Click The Links Below To View Documents Related To Prior Authorization Requirements.
• current (up to 6 months), adequate patient history related to the requested. Change office location, hours, phone, fax, or email. Web prior authorization is not a guarantee of payment for services. If prior authorization is needed for a certain service, your provider must get it before giving you the service.
Add Or Terminate A Provider.
Add or close a location. 2023 medicaid pa guide/request form (vendors) effective 07.01.2023 important information for molina healthcare medicaid providers information generally required to support authorization decision making includes: Items on this list will only be dispensed after prior authorization from molina healthcare. The forms are also available on the frequently used forms page.