Wellcare By Allwell Prior Auth Form
Wellcare By Allwell Prior Auth Form - Pharmacy policies & forms coverage determinations and. Web prior authorization, step therapy, & quantity limitations; Web prior authorization, step therapy, & quantity limitations; Prior authorization, step therapy, & quantity limitations; Login or create a secure portal account; Web pharmacy policies & forms coverage determinations and redeterminations. Web authorizations providers must obtain prior authorization for certain services and procedures. Our family of products is growing! Web prior authorization, step therapy and quantity limits. Web find out more about becoming a wellcare by allwell from mhs contracted provider.
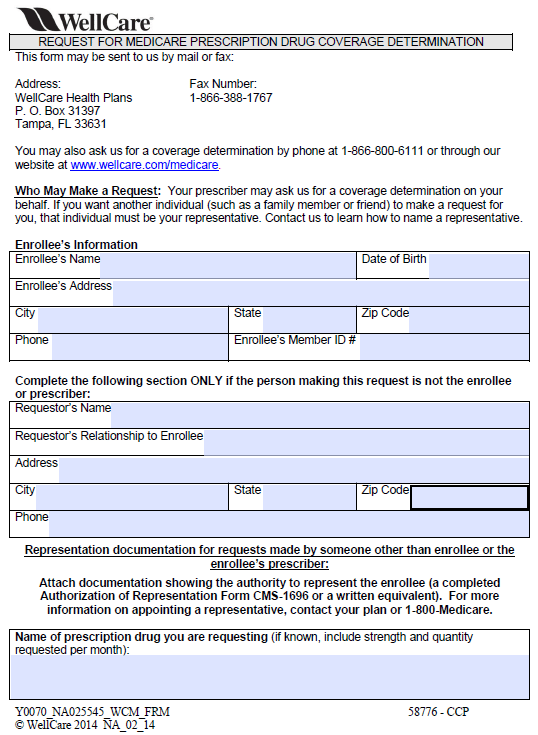
Pharmacy policies & forms coverage determinations and. Complex imaging, mra, mri, pet and ct scans need to be verified. Web fill out and submit this form to request prior authorization (pa) for your medicare prescriptions. Web pharmacy policies & forms coverage determinations and redeterminations. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. Web prior authorization, step therapy, & quantity limitations; Web wellcare prior (rx) authorization form. A wellcare prior authorization form is a document used for requesting certain. Web authorization lookup please select your line of business and enter a cpt code to look up authorization for services.
Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. Web wellcare prior (rx) authorization form. Web prior authorization, step therapy, & quantity limitations; Web wellcare by allwell provider. Web authorization lookup please select your line of business and enter a cpt code to look up authorization for services. Web prior authorization, step therapy and quantity limits. Pharmacy policies & forms coverage determinations and. Web authorizations providers must obtain prior authorization for certain services and procedures. Prior authorization, step therapy, & quantity limitations; Web up to $40 cash back edit wellcare prior authorization form.
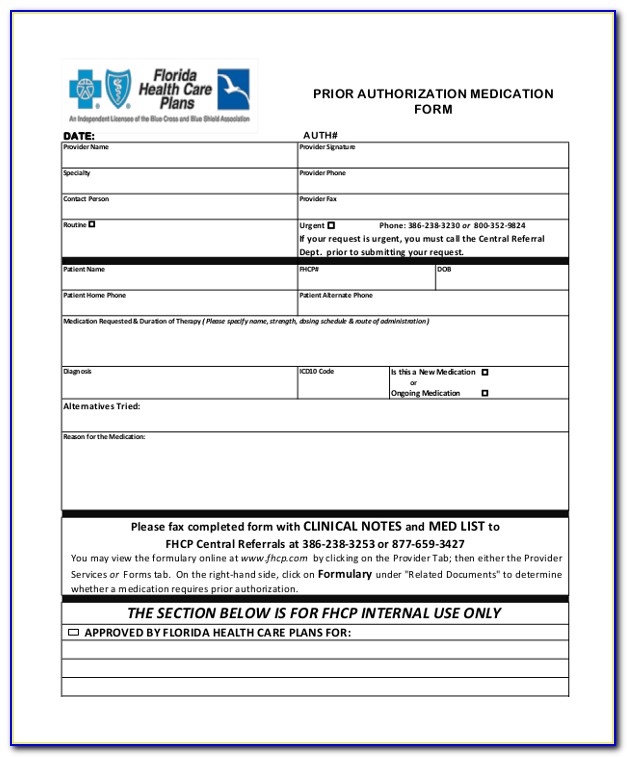
Medicare Part D Prior Authorization form for Medication Lovely Wellcare
Web pharmacy policies & forms coverage determinations and redeterminations. Web pharmacy forms & notices. Web find out more about becoming a wellcare by allwell from mhs contracted provider. While we’ll cover some of that information in this presentation, your toolkit has additional information including: Authorization requirements are available in the quick reference guide.
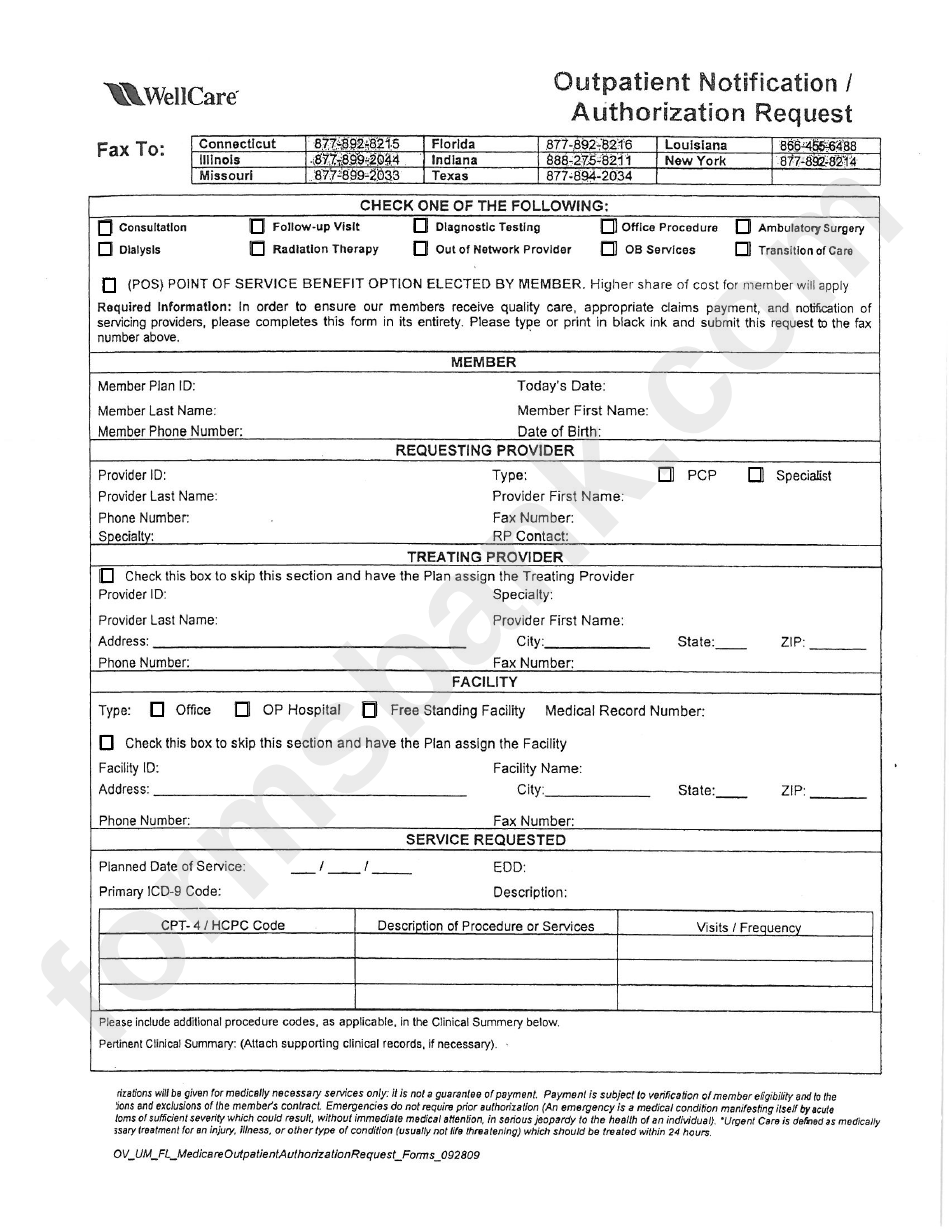
Fillable Outpatient Notification /authorization Request Wellcare
Web wellcare by allwell provider. During this process, we may request. Authorization requirements are available in the quick reference guide. Web pharmacy forms & notices. Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit.
Wellcare Medicare Medication Prior Authorization Form Form Resume
Web find out more about becoming a wellcare by allwell from mhs contracted provider. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Web the prior authorization span for elective inpatient admissions will be increased to 60 (sixty) days for dates of service on or after 11/1/2022. Web pharmacy policies &.
Wellcare prior authorization form Fill out & sign online DocHub
Web up to $40 cash back edit wellcare prior authorization form. Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Web wellcare prior (rx) authorization form. Web fill out and submit this form to request prior authorization (pa) for your medicare prescriptions. However, this does not guarantee.
Credentialing Application Template Master of Documents
Pharmacy policies & forms coverage determinations and. Web authorization lookup please select your line of business and enter a cpt code to look up authorization for services. Web pharmacy forms & notices. Web prior authorization, step therapy and quantity limits. Web the prior authorization span for elective inpatient admissions will be increased to 60 (sixty) days for dates of service.
ads/responsive.txt Wellcare Prior Auth form Medication Beautiful Family
Add and change text, add new objects, move pages, add watermarks and page numbers, and more. If you have questions about. Web pharmacy policies & forms coverage determinations and redeterminations. Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Web wellcare is the medicare brand for centene corporation,.
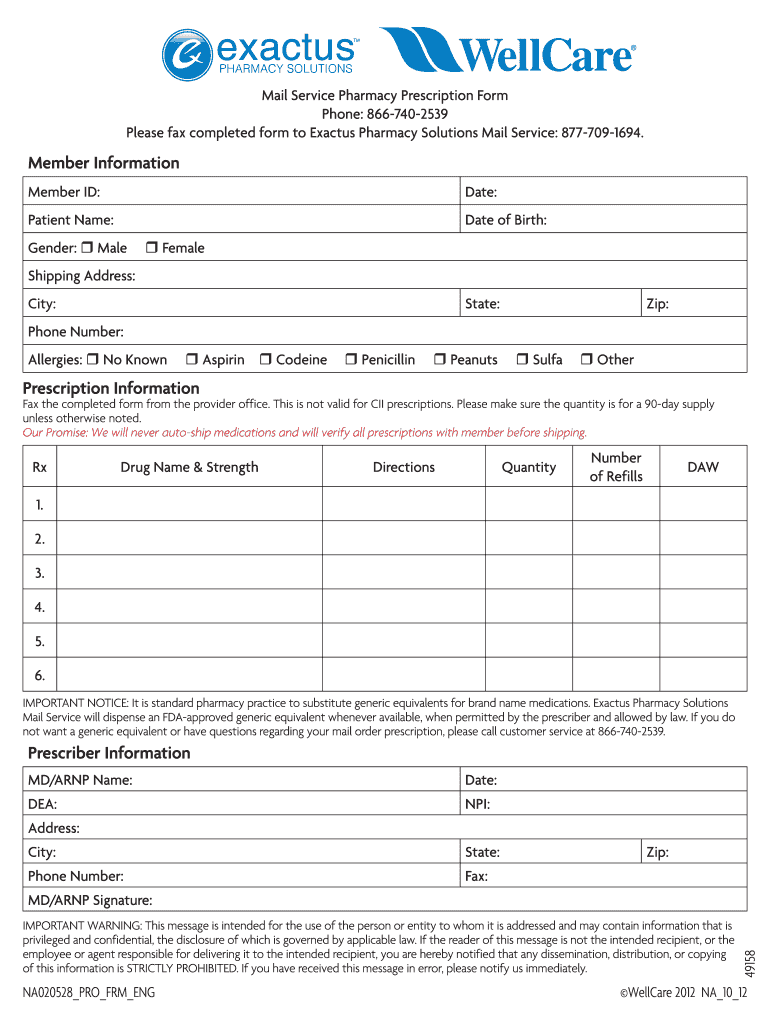
Wellcare NA020528 2012 Fill and Sign Printable Template Online US
Prior authorization, step therapy, & quantity limitations; Our family of products is growing! Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. While we’ll cover some of that information in this presentation,.
Prior authorization form for caremark
Medicare advantage plans offered through wellcare by allwell can be accessed on their website. Select the document you want to sign and click upload. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Web authorization lookup please select your line of business and enter a cpt code to look up authorization.
Medco Health Medicare Part D Prior Auth Form Form Resume Examples
Web pharmacy policies & forms coverage determinations and redeterminations. Prior authorization, step therapy, & quantity limitations; Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Web prior authorization, step therapy,.
How To Submit Pre Authorization To Medicare
Web prior authorization, step therapy, & quantity limitations; • welcome letter • secure portal setup. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Web if you are uncertain that prior authorization is needed, please submit a request for an accurate response. Here’s a list of pharmacy documents and forms you may need.
If You Have Questions About.
During this process, we may request. Web wellcare is the medicare brand for centene corporation, an hmo, ppo, pffs, pdp plan with a medicare contract and is an approved part d sponsor. Select line of business select enter cpt. A wellcare prior authorization form is a document used for requesting certain.
Web If You Are Uncertain That Prior Authorization Is Needed, Please Submit A Request For An Accurate Response.
Login or create a secure portal account; Select the document you want to sign and click upload. Our family of products is growing! If the planned admission date.
Web Authorization Lookup Please Select Your Line Of Business And Enter A Cpt Code To Look Up Authorization For Services.
Here’s a list of pharmacy documents and forms you may need when using your medicare part d benefit. Web find out more about becoming a wellcare by allwell from mhs contracted provider. Web pharmacy forms & notices. Web wellcare by allwell provider.
Web Prior Authorization, Step Therapy, & Quantity Limitations;
Medicare advantage plans offered through wellcare by allwell can be accessed on their website. Pharmacy policies & forms coverage determinations and. Web pharmacy policies & forms coverage determinations and redeterminations. Web authorizations providers must obtain prior authorization for certain services and procedures.